Yes, Good Irritable Bowel Syndrome Do Exist
Yes, Good Irritable Bowel Syndrome Do Exist
Blog Article
Effective Strategies for Recovering Irritable Bowel Syndrome (IBS).
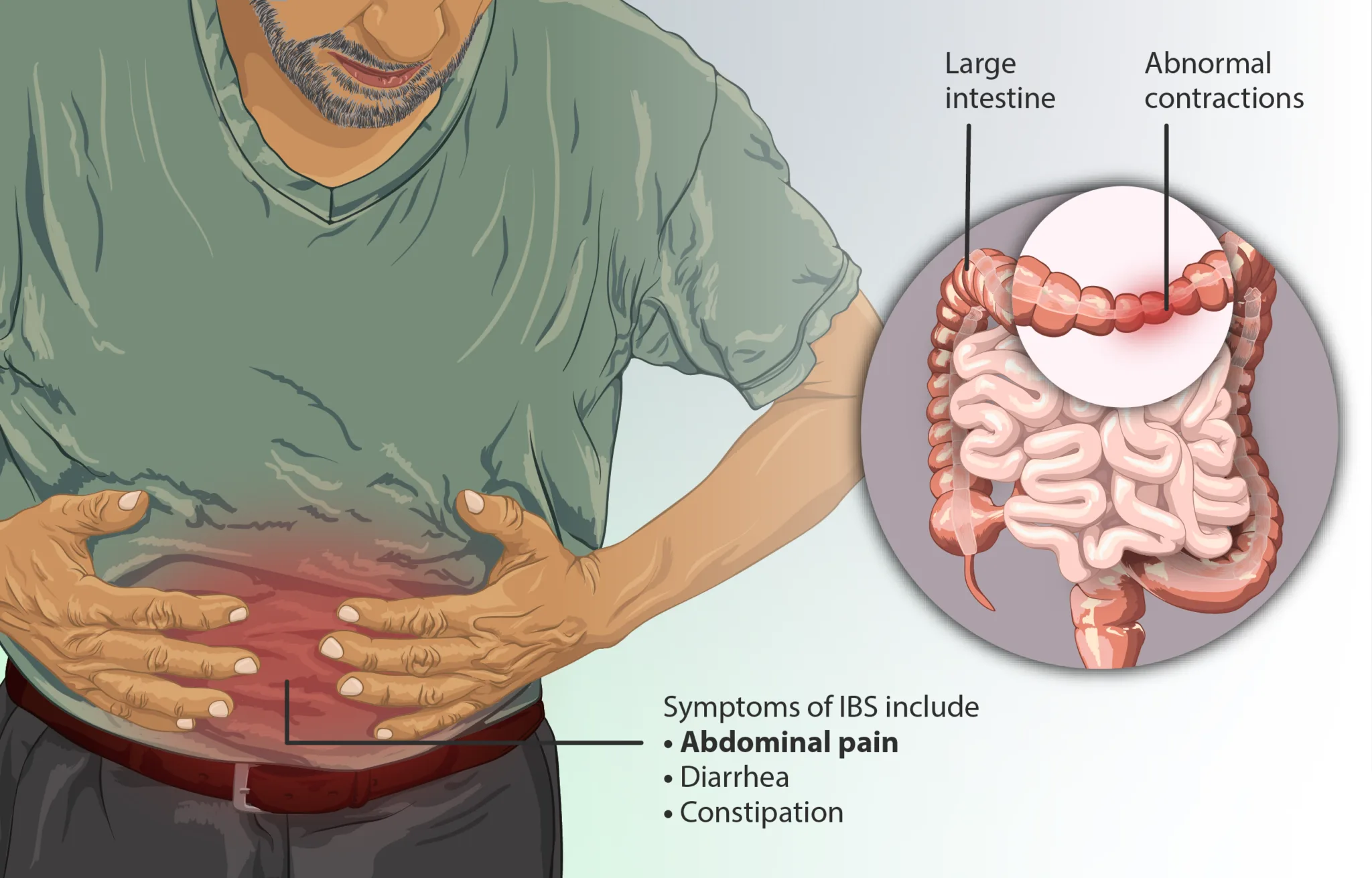
Irritable Bowel Syndrome (IBS) is a common gastrointestinal condition that affects millions of people worldwide, identified by symptoms such as bloating, abdominal discomfort, irregularity, diarrhea, and irregular bowel movements. In spite of being a widespread condition, the exact causes of IBS stay evasive, making it a complex syndrome to handle. This disorder, which is frequently persistent, can interfere with the daily life of those affected, as it hinders food digestion and triggers considerable discomfort. While numerous look for standard treatments like medication or dietary modifications, a growing number of people are turning to root cause methods to recover IBS from within, concentrating on long-lasting solutions rather than symptom management alone.
At the core of managing IBS efficiently is comprehending that it is not simply an intestinal concern. Instead, it often stems from a combination of elements such as gut dysbiosis, stress, food level of sensitivities, and way of life practices. An origin technique includes recognizing these underlying aspects and resolving them straight, permitting more enduring relief and recovery.
Gut Health and IBS.
The health of the gut microbiome is elaborately connected to IBS. Our gut is home to trillions of germs, much of which are necessary for food digestion, nutrient absorption, and total immune function. Nevertheless, an imbalance in these germs, typically described as "gut dysbiosis," can add to the beginning and progression of IBS symptoms. Restoring balance in the gut is, therefore, one of the first steps towards recovery the condition.
One method to begin this process is by incorporating probiotics and prebiotics into the diet. Probiotics are beneficial germs that can assist bring back balance in the gut microbiome, while prebiotics serve as food for these bacteria, helping them flourish. Many people with IBS have actually reported enhancements in their symptoms after consistently taking probiotics and ensuring their diet plan supports gut health. Foods abundant in probiotics consist of yogurt, kefir, and fermented vegetables like sauerkraut. Prebiotic-rich foods include bananas, garlic, onions, and asparagus.
In addition to probiotics, dietary modifications can considerably impact gut health. An elimination diet plan, which includes eliminating potential trigger foods and slowly reestablishing them, can help identify particular food level of sensitivities or intolerances that might be contributing to IBS signs. Typical triggers for those with IBS include gluten, dairy, and certain kinds of carbs known as FODMAPs. A low-FODMAP diet plan, which includes decreasing foods high in fermentable carbs, has actually been widely acknowledged as an efficient dietary strategy for managing IBS.
Tension and the Gut-Brain Connection.
The gut-brain axis is a bidirectional communication system in between the gut and the brain. This connection plays a significant function in the manifestation of IBS symptoms. Tension and anxiety can worsen IBS, resulting in flare-ups and intensifying digestion problems. The nervous system, especially the vagus nerve, directly affects gut motility and sensitivity. For that reason, dealing with tension is essential when it pertains to managing and recovery IBS.
Mind-body practices such as mindfulness meditation, yoga, and deep breathing exercises IBS have actually shown pledge in decreasing the intensity of IBS symptoms by relaxing the nervous system. These practices can help in reducing stress, promote relaxation, and enhance gut function over time. Regular exercise also contributes in reducing tension levels and promoting healthy food digestion.
Integrating tension management techniques into life can have extensive effects on gut health and total well-being. For example, cognitive-behavioral treatment (CBT), a form of psychotherapy, has actually been used efficiently in individuals with IBS to help them handle stress and develop coping systems for their signs. This approach highlights the significance of resolving not just the physical aspects of IBS however likewise the psychological and psychological parts.
Hormonal Influence on IBS.
For some individuals, hormonal imbalances can contribute in activating or worsening IBS symptoms. Ladies, in particular, might notice changes in their gastrointestinal health around their menstruation. Variations in estrogen and progesterone can affect gut motility, resulting in either constipation or diarrhea. During specific times of the menstruation, IBS signs might become more pronounced, particularly in those who are currently inclined to the condition.
Resolving hormone imbalances through natural methods such as dietary changes, herbal supplements, and lifestyle modifications can help reduce their influence on IBS. For example, stabilizing blood sugar level levels, improving sleep quality, and reducing inflammatory foods from the diet can contribute to better hormonal policy. Herbal supplements like chasteberry or evening primrose oil may also help support hormonal balance, though it's essential to speak with a healthcare provider before starting any supplementation.
Inflammation and IBS.
Chronic inflammation in the gut can be another key contributor to IBS symptoms. Inflammation can damage the lining of the gut, causing increased intestinal permeability, often described as "dripping gut." When the gut lining is jeopardized, contaminants and undigested food particles can travel through the digestive wall, setting off an immune reaction that results in further inflammation and digestive distress.
Recovering the gut lining is an essential part of addressing IBS at its root. Nutrients like L-glutamine, an amino acid that supports the repair work of the gut lining, can be helpful for those with IBS. In addition, integrating anti-inflammatory foods into the diet, such as turmeric, ginger, and omega-3 fatty acids, can help reduce swelling and promote gut recovery.
Decreasing inflammation through way of life modifications is also important. Persistent tension, poor sleep, and a sedentary way of life can all add to increased inflammation in the body. By adopting a more well balanced way of life, individuals with IBS can help mitigate the results of inflammation and improve their total gastrointestinal health.
A Personalized Approach to Healing IBS.
One of the obstacles of dealing with IBS is that there is no one-size-fits-all solution. Every individual with IBS might have various triggers, symptoms, and underlying causes. For that reason, a personalized method to healing IBS is essential. Working with a health care professional or a practical medicine specialist can help recognize specific aspects adding to IBS and create a customized treatment plan.
This plan might include a mix of dietary changes, tension management methods, gut-healing protocols, and supplements. By addressing the origin of IBS, individuals can work towards long-term relief instead of just handling symptoms.
In addition, testing for food sensitivities, hormonal agent levels, and gut health markers can provide important insights into the specific areas that require attention. For example, testing for little intestinal bacterial overgrowth (SIBO) can assist recognize whether an overgrowth of bacteria in the small intestine is adding to IBS symptoms. Attending to SIBO with targeted treatment, such as antibiotics or herbal antimicrobials, can result in significant improvements in gut health.
Conclusion.
Recovering Irritable Bowel Syndrome (IBS) requires a holistic method that surpasses merely dealing with symptoms. By focusing on the origin of the disorder, such as gut dysbiosis, stress, hormone imbalances, and swelling, individuals can accomplish long-lasting relief and enhanced digestive health. While the journey to recovery might take time and effort, attending to these underlying aspects through dietary changes, stress management, and personalized care can cause lasting improvements. Dealing with health care professionals to tailor a plan that fits your special needs can make all the difference in managing IBS successfully. Through a dedication to lifestyle changes and comprehending the intricacy of the gut-brain connection, it is possible to regain control over your digestive health and lead a more comfortable, symptom-free life. Report this page